anatomy and physiology of heart pdf
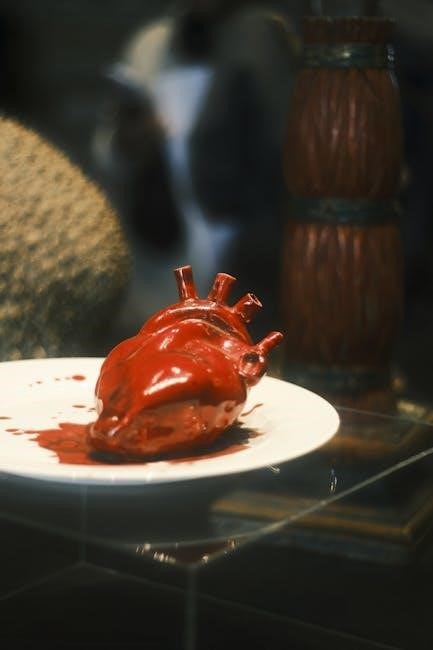
The heart is a muscular organ in the central chest cavity, functioning as a pump for blood circulation. It consists of four chambers and valves, ensuring one-way blood flow through pulmonary and systemic circuits, essential for oxygen delivery and overall bodily function.
1.1 Definition and Overview
The heart is a muscular organ located in the chest cavity, functioning as a pump for the circulatory system. It consists of four chambers and valves, enabling one-way blood flow through pulmonary and systemic circuits. This organ is essential for delivering oxygen-rich blood to tissues and returning deoxygenated blood to the lungs, ensuring efficient bodily function and survival.
1.2 Importance of the Heart in the Circulatory System
The heart is central to the circulatory system, acting as a pump to maintain continuous blood flow. It ensures oxygen-rich blood is delivered to tissues and organs while returning deoxygenated blood to the lungs for oxygenation. Without the heart, the body cannot sustain life, as cells depend on this system for nutrient delivery and waste removal, making it indispensable for overall health and function.

Gross Anatomy of the Heart
The heart is a muscular organ in the chest cavity, about the size of a fist, located in the mediastinum, surrounded by membranes, with a conical shape.
2.1 Location and Position in the Thoracic Cavity
The heart is centrally located in the thoracic cavity within the mediastinum, a region between the lungs. It is tilted, with the right side facing downward and the apex pointing to the left. The heart is surrounded by the pericardium and protected by the ribcage. Its position allows efficient blood circulation throughout the body, supported by nearby structures like the trachea, esophagus, and lymph nodes.
2.2 Size, Shape, and External Features
The heart is approximately the size of a closed fist, weighing about 250-300 grams. It is conical in shape, with the broad base at the top and the apex at the bottom. External features include the auricles, coronary arteries, and veins. The coronary sulcus separates the atria from the ventricles, and the heart is encased in a double-layered membrane called the pericardium, aiding in smooth functioning.
2.3 Layers of the Heart Wall
The heart wall consists of three layers: the epicardium, myocardium, and endocardium. The epicardium is the outermost layer, protecting the heart. The myocardium is the thick, muscular middle layer enabling contraction. The endocardium lines the inner surfaces, including the chambers and valves, ensuring smooth blood flow. These layers work together to maintain cardiac structure and function effectively.

Chambers of the Heart
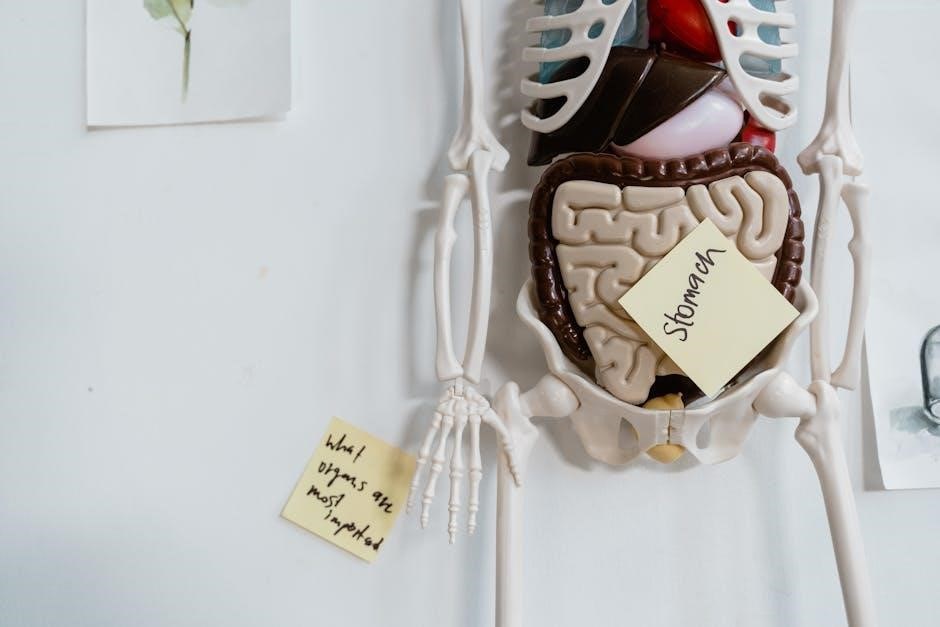
The heart has four chambers: right atrium, right ventricle, left atrium, and left ventricle. They work together to pump blood efficiently through the body.
3.1 Right Atrium and Right Ventricle
The right atrium receives deoxygenated blood from the venae cavae and coronary sinus, functioning as the initial receiving chamber. The right ventricle, receiving blood from the right atrium via the tricuspid valve, pumps it to the lungs through the pulmonary artery for oxygenation. Together, they ensure efficient blood circulation between the body and the lungs.
3.2 Left Atrium and Left Ventricle
The left atrium receives oxygen-rich blood from the pulmonary veins and transfers it to the left ventricle through the mitral valve. The left ventricle, the strongest chamber, pumps blood through the aortic valve into the aorta, supplying oxygenated blood to the body. Its thicker walls handle higher pressure for systemic circulation, ensuring efficient oxygen delivery to tissues and organs.
3.3 Septa and Their Functions
The heart contains two septa: the atrial septum, which separates the right and left atria, and the ventricular septum, dividing the right and left ventricles. These septa prevent blood mixing between the chambers and ensure proper directional flow. The atrial septum includes the foramen ovale in the fetus, which closes after birth. The ventricular septum is thicker, supporting higher pressures in the ventricles.
Valves of the Heart
The heart contains four valves—tricuspid, pulmonary, mitral, and aortic—each ensuring unidirectional blood flow, preventing backflow, and maintaining efficient circulation throughout the body.
4.1 Atrioventricular Valves
The atrioventricular valves, including the tricuspid and mitral valves, are located between the atria and ventricles. They consist of leaflets (cusps) attached to the valve annulus. These valves ensure blood flows only in one direction, from the atria to the ventricles, during ventricular systole. The chordae tendineae and papillary muscles prevent valve prolapse, maintaining proper closure and preventing regurgitation, ensuring efficient blood flow through the heart.
4.2 Semilunar Valves
The semilunar valves, comprising the pulmonary and aortic valves, are situated at the bases of the pulmonary artery and aorta. These valves consist of three cusps that open during ventricular systole, allowing blood to flow into the pulmonary and systemic circulations. They close during diastole to prevent backflow into the ventricles, ensuring unidirectional blood flow. Their proper function is crucial for maintaining efficient circulation;
4.3 Mechanism of Valve Function
The heart valves function through pressure gradients and mechanical forces. During systole, ventricular pressure exceeds arterial pressure, opening the semilunar valves. Conversely, during diastole, lower ventricular pressure allows the atrioventricular valves to open. Papillary muscles and chordae tendineae stabilize the valves, preventing prolapse. This synchronized mechanism ensures unidirectional blood flow, maintaining efficient circulation and preventing backflow, which is vital for cardiac efficiency and overall health.
Blood Circulation Through the Heart
The heart facilitates blood circulation by receiving deoxygenated blood in the right atrium, pumping it to the lungs for oxygenation, and returning oxygenated blood to the body. Coronary circulation ensures the heart muscle itself is supplied with oxygen and nutrients, maintaining its functionality and overall cardiovascular health.
5.1 Pulmonary Circulation
Pulmonary circulation begins when deoxygenated blood from the right ventricle flows through the pulmonary artery to the lungs. In the alveolar capillaries, oxygen diffuses into the blood, and carbon dioxide is removed. Oxygenated blood returns to the heart via the pulmonary veins, entering the left atrium. This pathway ensures efficient gas exchange, essential for cellular respiration and overall bodily function.
5.2 Systemic Circulation
Systemic circulation delivers oxygenated blood from the left ventricle to the body via the aorta. Arteries distribute blood to tissues, where oxygen and nutrients diffuse into cells, and carbon dioxide and waste products are collected. Deoxygenated blood returns through veins to the right atrium, completing the cycle. This pathway is vital for supplying oxygen and nutrients to tissues, supporting cellular functions, and maintaining overall health.
5.3 Coronary Circulation
Coronary circulation supplies oxygenated blood to the myocardium, the heart muscle itself. The coronary arteries originate from the aorta and branch into the right and left coronary arteries. These vessels distribute blood to the atria and ventricles, ensuring cardiac cells receive oxygen and nutrients. The coronary sinus collects deoxygenated blood, returning it to the right atrium. This circulation is vital for maintaining heart function and overall cardiac health.
Cardiac Conduction System
The cardiac conduction system regulates heartbeat rhythm, ensuring coordinated contractions. It includes the SA node, AV node, Bundle of His, bundle branches, and Purkinje fibers, maintaining a consistent rhythm.
6.1 Structure and Function of the Conduction Pathway
The cardiac conduction pathway consists of specialized cells that generate and transmit electrical impulses. It includes the sinoatrial (SA) node, atrioventricular (AV) node, Bundle of His, bundle branches, and Purkinje fibers. These components work sequentially to initiate and coordinate contractions, ensuring a synchronized heartbeat. The pathway is crucial for maintaining a consistent heart rhythm and proper cardiac function.
6.2 Role of the Sinoatrial (SA) Node
The sinoatrial (SA) node, located in the right atrium, acts as the heart’s natural pacemaker. It generates electrical impulses at a rate of 60-100 beats per minute, setting the heart’s rhythm. These impulses trigger atrial contractions, ensuring a consistent and synchronized heartbeat. The SA node’s intrinsic rate is influenced by the autonomic nervous system, balancing heart activity with bodily needs.
6.3 Electrical Conduction and Its Regulation
The electrical conduction system regulates heartbeat rhythm through a coordinated pathway. The impulse travels from the SA node to the atria, causing contraction, then to the AV node, introducing a delay. It proceeds through the Bundle of His, bundle branches, and Purkinje fibers, triggering ventricular contractions. The autonomic nervous system fine-tunes this process, balancing sympathetic and parasympathetic inputs to adapt heart rate to physiological demands.

Cardiac Cycle and Heart Sounds
The cardiac cycle comprises phases of isovolumetric contraction, rapid ejection, reduced ejection, isovolumetric relaxation, rapid filling, and diastasis. Heart sounds S1 and S2 result from valve closures.
7.1 Phases of the Cardiac Cycle
The cardiac cycle consists of two main phases: systole (contraction) and diastole (relaxation). Systole includes isovolumetric contraction, rapid ejection, and reduced ejection. Diastole involves isovolumetric relaxation, rapid filling, and diastasis. These phases ensure efficient blood pumping and chamber filling, maintaining cardiac efficiency and proper blood circulation throughout the body.
7.2 Origin and Significance of Heart Sounds
Heart sounds originate from valve closures and blood flow turbulence. The first sound (“lub”) occurs during atrioventricular valve closure, while the second sound (“dub”) results from semilunar valve closure. These sounds are crucial for assessing cardiac function and detecting abnormalities like murmurs, which may indicate valve disorders or congenital heart defects, aiding in early diagnosis and treatment.

Cardiac Physiology
Cardiac physiology studies the heart’s functional processes, including muscle contraction, electrical activity, and blood flow regulation, ensuring efficient circulation and overall bodily health.
8.1 Cardiac Muscle Cells and Their Function
Cardiac muscle cells, or cardiomyocytes, are specialized cells with intercalated discs and T-tubules, enabling synchronized contractions. They generate force for pumping blood through striated muscle fibers and are rich in mitochondria for energy. These cells are uniquely adapted for endurance, ensuring continuous heart function without fatigue, making them central to the heart’s role in circulation and maintaining life-sustaining blood flow.
8.2 Regulation of Cardiac Contractility
The regulation of cardiac contractility involves the autonomic nervous system, where the sympathetic division enhances contractility via norepinephrine, and the parasympathetic division reduces it through acetylcholine. Hormones such as adrenaline increase contractility, while beta-blockers and certain calcium channel blockers decrease it. Intrinsic mechanisms, including the Frank-Starling law and calcium ion concentration within cardiomyocytes, also significantly influence the heart’s contractile force to meet physiological demands.
8.3 Autonomic Nervous System Control
The autonomic nervous system regulates heart function through sympathetic and parasympathetic branches. The sympathetic nervous system increases heart rate and contractility via norepinephrine, preparing the body for stress. The parasympathetic nervous system, primarily through the vagus nerve, releases acetylcholine to slow heart rate and promote relaxation. This dual control maintains cardiac homeostasis, adapting to physiological demands efficiently.
Clinical Examination of the Heart
Clinical examination of the heart involves inspection, palpation, auscultation, and blood pressure measurement. These assessments help evaluate cardiac function, detect abnormalities, and guide further diagnostic procedures effectively.
9.1 Inspection and Palpation
Inspection involves observing chest deformities, jugular venous distension, or abnormal pulsations. Palpation assesses chest vibrations, thrills, and heart sounds. These methods help identify structural or functional heart abnormalities, guiding further clinical evaluation and ensuring accurate diagnosis of cardiac conditions.
9.2 Auscultation of Heart Sounds
Auscultation involves listening to heart sounds using a stethoscope to assess cardiac function. Normal sounds include S1 (atrioventricular valve closure) and S2 (semilunar valve closure). Additional sounds like S3 or murmurs may indicate abnormalities. This method provides critical insights into valve function, rhythm, and potential pathologies, aiding in the early detection of heart conditions.
9.3 Measurement of Blood Pressure
Measuring blood pressure involves assessing the force of blood against arterial walls using a sphygmomanometer. The systolic pressure (during heart contraction) and diastolic pressure (at rest) are recorded. Normal blood pressure typically ranges around 120/80 mmHg. Regular monitoring helps detect hypertension or hypotension, which are critical for diagnosing cardiovascular conditions and managing overall heart health effectively.
Diagnostic Techniques
Diagnostic techniques assess heart health. Key methods include ECG for electrical activity, echocardiography for imaging, and cardiac catheterization for blood flow analysis. These methods help diagnose various heart conditions effectively.
10.1 Electrocardiogram (ECG)
An electrocardiogram (ECG) is a non-invasive tool that measures the heart’s electrical activity. It uses electrodes placed on the chest to record voltage changes, creating a waveform. The PQRST complex represents depolarization and repolarization of atria and ventricles. ECG helps diagnose arrhythmias, ischemia, and infarction. It is painless, quick, and essential for assessing cardiac function and rhythm abnormalities in clinical settings.
10.2 Echocardiography
Echocardiography uses high-frequency sound waves to create images of the heart. It assesses chamber size, valve function, and blood flow. Types include transthoracic (external) and transesophageal (internal) echocardiograms. Doppler technology measures blood velocity, detecting abnormalities like stenosis or regurgitation. This non-invasive tool aids in diagnosing heart diseases, guiding treatments, and monitoring cardiac conditions effectively in clinical and diagnostic settings.
10.3 Cardiac Catheterization
Cardiac catheterization involves inserting a catheter into a blood vessel to access the heart. It diagnoses coronary artery disease, measures cardiac pressures, and assesses heart function. Techniques like angiography visualize coronary arteries, while interventions such as angioplasty or stent placement treat blockages. This procedure provides detailed insights, aiding in precise diagnosis and treatment of cardiovascular conditions, guided by imaging technologies.

Key Points and Summary
The heart is a muscular organ with four chambers, regulating blood flow through valves and the cardiac cycle. Its anatomy and physiology ensure efficient circulation and oxygen delivery, crucial for overall health and bodily functions.
11.1 Major Components of the Heart
The heart consists of four chambers: the right atrium, left atrium, right ventricle, and left ventricle. It also includes valves (atrioventricular and semilunar), the cardiac conduction system, and the heart wall layers (epicardium, myocardium, and endocardium). These components work together to ensure efficient blood circulation, oxygen delivery, and overall cardiac function, forming the structural and functional foundation of the cardiovascular system.
11.2 Integration of Anatomy and Physiology
The heart’s anatomy and physiology are intricately linked, with structures like chambers, valves, and the conduction system working in harmony to ensure blood circulation. Understanding how these components function together is essential for grasping heart dynamics and addressing clinical conditions, illustrating the seamless integration of form and function in maintaining cardiovascular health.
References and Further Reading
Key references include Berne & Levy Physiology and Harrison’s Principles of Internal Medicine. Journals like Circulation and Nature Reviews Cardiology provide cutting-edge research. Online access via ScienceDirect and university libraries offers comprehensive study materials.
12.1 Recommended Textbooks and Journals
Recommended textbooks include “Gray’s Anatomy” and “Guyton and Hall Textbook of Medical Physiology”. Journals like “Circulation” and “Journal of Physiology” provide in-depth insights. These resources are available in digital formats, including PDFs, and are essential for students and professionals studying cardiology and physiology.
12.2 Online Resources for Detailed Study
For detailed study, online resources like Coursera’s “Anatomy and Physiology” courses and Khan Academy’s heart anatomy tutorials are invaluable. Websites such as AnatomyTOOL and Visible Body offer 3D heart models. The American Heart Association provides downloadable PDF guides, while Google Scholar and NCBI host research papers for in-depth learning.